Wyandotte County cases rise to 34
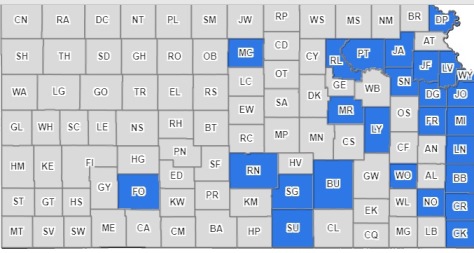
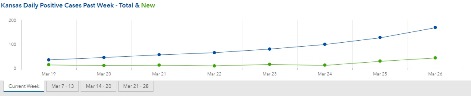
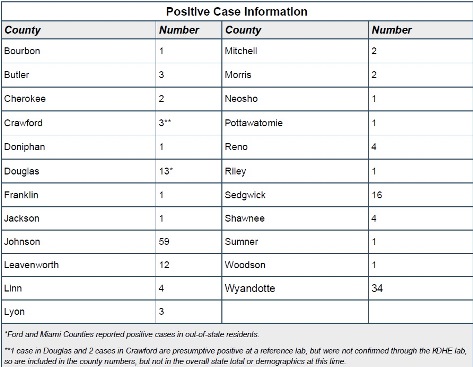
The number of positive cases of COVID-19 in Kansas increased from 126 on March 25 to 168 on March 26, according to a report from the Kansas Department of Health and Environment.
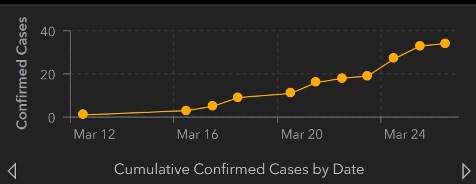
Positive cases in Wyandotte County increased from 27 on Wednesday to 34 on Thursday, according to the 11 a.m. KDHE report. Nineteen Wyandotte County patients were hospitalized, according to the UG website. Most patients have recovered; there were two deaths associated with COVID-19 in Wyandotte County.
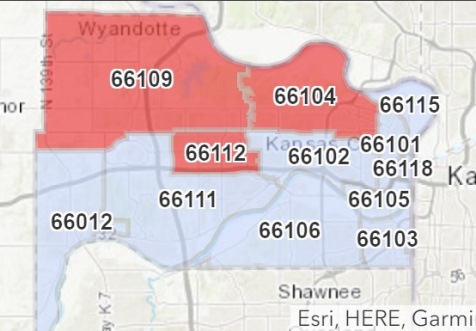
The UG’s COVID-19 website reported cases by Zip Code, with 8 cases in 66109, 6 cases in 66112 and 9 cases in 66104. The other Zip Code areas of Wyandotte County had less than 5 per area, and so numbers were not reported.
Johnson County’s total of positive COVID-19 cases went from 44 on Wednesday to 59 on Thursday, the report stated.
In Sedgwick County, the Wichita area, the total was 11 on Wednesday and 16 on Thursday, according to the report.
Leavenworth County now is at 12 total cases, and it was 11 on Wednesday. Douglas County, including the Lawrence area, went from 10 cases on Wednesday to 13 on Thursday.
According to state statistics, 90 of the positive cases were males and 78 were females. Patients were 7 to 90 years old, with the median age at 54. Around 4.5 percent of those persons who were tested, and all of them were ill, were positive for COVID-19, officials said on Wednesday.
“We are on the curve and how big that curve grows is entirely in the public’s hands,” Dr. Steve Stites, chief medical officer at the University of Kansas Health System, said during a teleconference on Thursday.
“There is no question that shelter at home works,” Dr. Stites said.
He cited New Rochelle, N.Y., which had 108 cases around March 12, started shutting down the city, and was at 200 cases two days ago. The prediction is this disease is doubling every two or three days, and they might have been at 1,000 if they hadn’t sheltered at home.
“We can do this, we can bend the curve,” he said. “We don’t want to be New York City, we want to be KC.”
He said he noticed 10-15 people gathered at a park last night, and wanted to tell them to stay home. Don’t go out in groups unless absolutely necessary, he said.
KU Hospital had 16 patients who were positive for COVID-19 on Thursday, he said, with eight or nine on mechanical ventilation.
“The numbers are increasing. We are on the front edge of the surge,” Dr. Stites said.
“In order to be successful and to beat COVID, which we can do, the most important player in this game is you,” he said. “It’s the people who are listening or reading and making the decision, do I stay at home. If you choose yes, we will bend that curve, and if you choose no, we will struggle. So the choice is what we do and what we make every day.”
Dr. Dana Hawkinson, medical director of infection prevention and control at the KU Health System, said he also saw a group of people last night, with the police trying to get a group dispersed and go back to their homes.
“People who continue to congregate and fail to stay home or maintain six feet apart are being irresponsible,” Dr. Hawkinson said.
In Wyandotte County, it is permissible under the “stay-home” ordinance to go to the parks and exercise, run or walk, keeping about six feet apart. Groups of 10 or more are prohibited.
“It was the police who were out there trying to get those people dispersed and back to their homes,” Dr. Hawkinson said. “It’s good to be out, but we don’t want the mass gatherings, because that’s how this virus is spread. We need to protect our first responders, including our police officers, because they’re the ones that do protect us. If we can stop the spread overall, we can stop the spread to our first responders, and that is the main goal of why we are trying to decrease the social gathering, to stay at home and stop the spread of this virus right now.”
Dr. Chad Cannon, Emergency Department chair at KU Health System, said he wanted to thank people for not coming in unnecessarily to the Emergency Department at KU Hospital. They continue to take care of the people having heart attacks, accidents and strokes, he said.
“We want to continue to have the capacity and the people to continue to take care of those folks, and we need to keep folks who are just concerned, but don’t have symptoms, out of the health care environment and home,” he said.
Those who have the COVID-19 serious symptoms, including fever, cough and shortness of breath, should call their health care providers first, he said.
Dr. Cannon said people should call their physician if they have shortness of breath, also if they have chest pain. If they are weak and fatigued and feel they are going to pass out, if they have altered mental state or confusion and slurred speech, they should consider the Emergency Department, he said. If they have a runny nose or cough without more severe symptoms, it doesn’t mean they don’t have coronavirus, but they should isolate themselves, call their physician and get further advice, before going anywhere, he said.
“We’re ready for this if the surge does come, and hopeful that if you heed this good advice, that the surge will be manageable and that we can flatten the curve,” he said.
Besides staying at home, doctors have stressed good hygiene practices, washing hands, covering a cough and cleaning frequently touched surfaces.
Dr. Stites also said he was hearing reports that health care workers at a large hospital in Wuhan, China, who had adequate personal protective equipment were staying healthy. COVID-19 spread to health care workers before they put in the protective equipment requirements, but afterward, they did not have a single case in the past six weeks, he said. The personal protective equipment requirements were the same used at KU Health System, he said.
Health care workers can still get COVID-19 in community spread, he said, but he doesn’t think they are getting the virus at the hospital.
At this time, KU Health System has adequate personal protective equipment, but they don’t know if it will be adequate in the next week or 10 days.
Some areas, such as New York, are short on protective equipment. Kansas City doesn’t want to go in that direction, Dr. Stites said.
To view the KU Health System news conference video, with more detailed information, visit https://www.medicalnewsnetwork.org/NewsNetwork/DocTalk/C/Coronavirus%20Media%20Conference%20Call%20March%2026%202020
The Kansas COVID-19 website is at
https://govstatus.egov.com/coronavirus.
The UG’s COVID-19 response website is at
https://alpha.wycokck.org/Coronavirus-COVID-19-Information.
COVID-19 information from the CDC is at https://www.cdc.gov/coronavirus/2019-nCoV/index.html.