As hospitals across the Kansas City area are filling up with COVID patients, chief medical doctors from several hospitals joined together Friday to ask residents to wear masks.
The doctors also encouraged everyone to get vaccinated.
“Hospitals are on the verge of a real crisis here because we do not have a lot more beds to give,” Dr. Steve Stites, chief medical officer of the University of Kansas Health System, said during a hospital CMO briefing on Friday hosted by the Greater Kansas City Chamber of Commerce.
Last fall, hospitals’ chief doctors went to the community and told them there was a problem with capacity with 270 COVID patients. Today, there are 376 COVID patients in area hospitals, Dr. Stites said.
“That’s a hundred more than when we came to you last time,” he said. “We are in the midst of a significant crisis.”
Last week, Kansas City, Missouri, implemented an indoor mask mandate for public spaces. On Thursday night, the Unified Government Commission passed an indoor mask mandate for public spaces, excluding schools and excluding Bonner Springs and Edwardsville. The UG Commission stated that those other governing bodies could make their own decisions on it.
Dr. James Stewart, chief medical officer at North Kansas City Hospital, said hospitals across the area are reporting they are full. When the hospitals are full and people get stuck in the emergency room waiting for a bed, it causes the emergency room to fill up, and the waiting room to fill up, he said.
The waiting time goes up, and a hospital then can go on a “high-volume status,” meaning the capacity of the emergency room is dangerously high. If more than half the hospitals in the region go on high-volume status, then the regional Health Care Coalition can force everyone to be open again, he said. That order has been rare in the past, he said. In July, the force open hours have been over 1,200 hours, he added.
They need to stay open for emergencies such as heart attacks and stroke, and other emergencies, and it’s getting tough to stay open with that, according to Dr. Stewart.
Dr. Stites said time is critical in heart attacks and strokes, with heart tissue or brain tissue destroyed if it is not treated in time.
“We’re struggling to get people taken care of,” he said. As the pandemic worsens, things will deteriorate inside the health systems, and they don’t want to see this, he added.
According to Dr. Mark Steele, executive chief clinical officer of Truman Medical Centers, when the Delta variant arrived, it resulted in a rapid rise in cases over the last three to four weeks, about a tenfold increase since the beginning of July. This has not been helped by lower vaccination rates and people out and about unmasked, he added.
With Delta, vaccinated people can carry viral loads of COVID similar to the unvaccinated, he said. The solution is to get everyone to wear a mask and to continue to chip away at getting more people vaccinated as quickly as they can, he said.
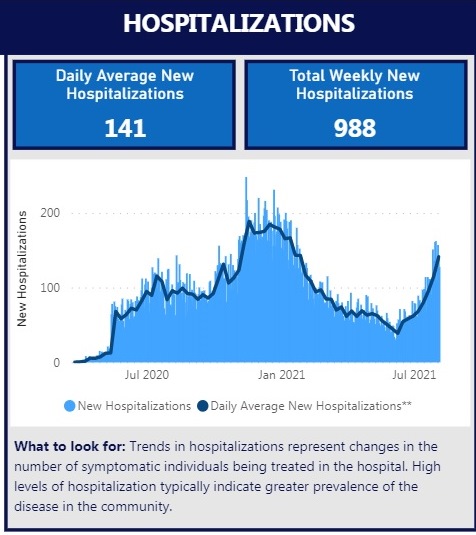
Dr. Stites said the seven-day average for the area has risen to a point that is now higher than it was on Nov. 5.
He said a lot of “elective surgeries” have already been moved to outpatient settings, and some are not really elective, but involve cancer and heart problems. The hospitals have the highest acuity cases.
Dr. Ahmad Barash, chief of staff, Kansas City VA Medical Center, said the Midwest is in a “hot” COVID area, with vaccination rates really low. The risk is from low vaccination rates and low numbers of people wearing masks.
Dr. Elizabeth Long, chief medical officer, Olathe Health System, said the average number of COVID hospitalizations in the metro area is going up, similar to January 2021. Typically COVID patients take a longer period of time in the hospital, not just two or three days, she said. Vaccinated patients tend to spend less time in the hospital.
Hospitals can’t take care of patients, can’t accept transfers and can’t transfer patients, she said. They have to implement a surge plan.
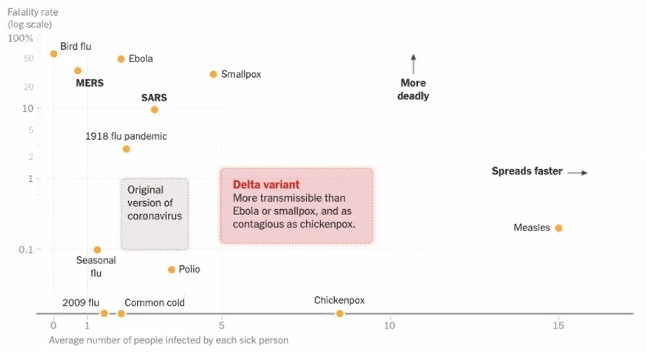
Dr. Raghu Adiga, chief medical officer, Liberty Hospital, said the transmissibility of the Delta variant is from 5 to 9, compared to the original COVID at 2. That means one infected Delta patient typically infects 5 to 9 other persons.
That percentage is close to the same infection rate as chicken pox.
People who carry Delta have about 10 times the amount of it in their respiratory tract, and carry it for a longer time, Dr. Adiga said.
Since it is more infectious, the mitigation measures need to be stronger, Dr. Adiga said.
The herd immunity needed for Delta is higher than the original COVID amount, according to Dr. Adiga.
Dr. Stites said 80 to 85 percent vaccination is needed to control the spread of the Delta variant.
Dr. Darryl Nelson, chief medical officer, HCA Midwest Health System, said 2,458 Greater Kansas City area residents have died from COVID. They are unequivocally impacted by vaccination, he said.
The concern is that this will be a continuing trend if they don’t make progress on vaccination and masking, he said.
Deaths from other disease are starting to show unfavorable trends as well, as some persons have delayed coming in for treatment.
Dr. Dana Hawkinson of KU Health System said there are also long-haul effects from COVID-19. A study found that 10 to 30 percent of COVID patients will experience post-infection conditions up to four months after infections.
Data from the 344 patients at the multi-disciplinary clinic for long haulers at KU Health showed that two patients sought six specialties for assistance; 12 of patients saw five; four had seen four specialties; 51 patients had seen three specialties; 98 patients saw two specialties; and 157 patients saw one specialty.
Dr. William Gilbirds, chief medical officer, Saint Luke’s Care, said 90 percent of hospitals report moderate to significant staffing concerns. Thirty-four percent of hospitals anticipate a shortage of staffing next week, he said.
“We need to take steps immediately to stop this transmission,” he said.
The hospitals are turning down transfers because they don’t have the capacity to take them, he said.
The doctors said that they can’t just hire more nurses because there is a shortage of available nurses, and the numbers choosing to go into the field are declining.
Dr. Jennifer Schrimsher, infectious disease specialist, Lawrence Memorial Hospital, said masking changes the course of the pandemic, and a third of infections can be prevented by masks.
“We’ve had no known cases of patient to staff transmission in our hospital,” she said.
A year ago, when experiencing the first real surge of patients, they were able to reduce cases t by a third by asking community members to mask when in public, she said. That is important again as they bring college students back to the campus.
With schools reopening in the fall, Dr. Jennifer Watts, director for emergency preparedness, Children’s Mercy Hospital, said they are seeing an increase in pediatric cases. Last week there were 269 COVID cases, both inpatients and outpatients, and 259 positive cases for RSV, she said.
They are expecting influenza to be here this winter, along with the other respiratory viruses, she said. They are a little concerned about where they will be in the winter, she added.
The top priority is for kids to be in school, for many reasons, and in order to do that they have to have mitigation strategies in place, she said. Masking, hand hygiene, cleaning all work, but when vaccination rates are low, it has to be increased.
The best thing for children is to cocoon them, she said, and vaccinate everyone around them. It offers a little more protection. They are hoping vaccinations become available for younger kids later this year. They strongly encourage vaccination for age 12 and older.
Until community rates drop, they recommend strong mitigation strategies in place to keep the schools open, she said.
Dr. Lisa Hays, chief medical officer, AdventHealth Shawnee Mission, talked about the “Swiss cheese model,” where one mitigation strategy might not work by itself, but all the things added together can prevent the virus. Distancing, hygiene, wearing masks, staying home when sick, avoiding time in crowds, testing, quarantining and isolating, and being vaccinated, are among many things that can be done.
“We need masking back,” Dr. Stites said. ”It would be great to get everybody vaccinated overnight, but it takes four to eight weeks before full effectiveness.
“There is only one mitigation strategy we’re aware of that could clearly work – masking clearly works,” he said. “We need everybody to wear a mask.”
Masking helps all the other patients, also, not just COVID patients, because it will help free beds to care for the other patients.
Doctors from 11 hospitals in the Greater Kansas City area all reported that their COVID-19 patient numbers had increased in the past several weeks. The increase is attributed to the Delta variant, which spreads more quickly. All the hospitals reported they were either at capacity or near capacity.
For example, St. Luke’s health system reported 129 positive COVID-19 patients across its health system, according to Dr. William Gilbirds. They are seeing increased numbers also from patients who delayed care earlier. The hospital work force has seen an effect from illness, with about 50 out from confirmed COVID, and they are trying to manage high volumes in the emergency department. St. Luke’s East is seeing a higher volume of COVID patients since the Fourth of July, including some from the Lake of the Ozarks region, with 94 percent unvaccinated, and nearly half of patients between 20 and 59.
The University of Kansas Health System in Kansas City, Kansas, reported 46 COVID-19 patients on Friday, with 10 in the intensive care unit and seven on ventilators, according to Dr. Steve Stites. There were 452 COVID-related deaths since the beginning of the pandemic, with 282 who died in the hospital. Of those, four were vaccinated and they were severely chronically ill. KU is not able to accept patients through transfers, and on Friday had 808 patients in the hospital. They are staffing alternate care areas, and there were 20 patients in the emergency room waiting for beds, he said.
HCA hospitals, including seven area hospitals, are seeing 145 COVID patients currently, with 46 in the intensive care unit and 24 on ventilators, according to Dr. Darryl Nelson. Research, Menorah and Overland Park are among these hospitals. Between 3 and 8 percent of COVID patients in the hospital have been vaccinated. They are managing, but uneasy about the trends. They are at 94 percent staff capacity, and the ICUs are at 95 percent capacity. They are right on the edge of the capacity situation.
Dr. Lisa Hays of AdventHealth reported COVID patients grew from eight in the beginning of July to 34 currently, with eight in the ICU and six on a ventilator. There are staffing shortages currently, and 15 employees were on quarantine from COVID. In July there were 26 employees out with COVID, and all but five were unvaccinated.
The Kansas City VA Hospital reported 14 inpatients with COVID, and four in the ICU, according to Dr. Ahmad Batrash. There were 100 outpatients active with COVID. The number of COVID patients has tripled in the past two weeks, he reported. Bed capacity is very tight, with only two ICU beds available and a couple of medical surge beds. Since the beginning of the pandemic, they have lost 77 veterans to COVID, with 68 deaths at the hospital and 18 outside. Of the deaths, only one patient was vaccinated. “We know the vaccine saves lives,” he said.
Truman Medical Center reported 55 COVID inpatients, compared to 20 on July 9, according to Dr. Mark Steele. In June the number was in the teens. The number now is very close to the high of 62 that was the winter peak, he said. Over 95 percent of the COVID patients have not been vaccinated. July saw 12 COVID-related deaths, with three-quarters of them in the last two weeks of July. None of the deaths was in fully vaccinated individuals. Staffing all available beds continues to be a challenge.
Children’s Mercy Hospital reported an all-time high Friday with 19 COVID inpatients, with seven in the ICU, according to Dr. Jennifer Watts. In the past few weeks there were about 30 new positive cases among employees per week, she said. Many patients are not yet eligible to receive the vaccine. There has also been an increase in viral illnesses including RSVs, she said, and they are running full most days.
North Kansas City hospital reported 72 COVID inpatients, with 13 in ICU and nine on ventilators, according to Dr. James Stewart. Ninety percent of the COVID patients are not vaccinated. None of the vaccinated COVID patients are currently in the ICU. Thirty-four employees are out now with COVID, up from 10 a few months ago. From the beginning of the pandemic, there were 283 deaths from COVID at the hospital.
Liberty Hospital reported 32 COVID inpatients with seven in the ICU and three on ventilators, according to Dr. Raghu Adiga. All but one patient was unvaccinated. Most patients are in their 50s, with one in the 20s and one in the 30s. Currently there are 17 staff members who are not working because of COVID. They have brought in extra staff to deal with overflow beds. They have had to go on diversion several times.
Olathe Medical Center and Miami County Medical Center reported they formerly had 0 to 4 COVID patients, and now are up to 25, with eight in the ICU and two on ventilators, according to Dr. Elizabeth Long. Nineteen percent of the COVID patients are vaccinated at Olathe, and 25 percent (one patient out of four) are vaccinated at Miami County. Those patients who are vaccinated have a decreased length of stay in the hospital and decreased acuity. Only one patient in the ICU was fully vaccinated, with chronic lung disease. Eleven employees were out with COVID, with less than half vaccinated. The ICU was absolutely full, and only one bed on the floor was open on Friday.
Lawrence Memorial Hospital reported seven COVID-19 patients on Friday, down from nine a few days ago, according to Dr. Jennifer Schrimsher. One was in the ICU and none on ventilators. Only one hospitalized COVID-19 patient was vaccinated. There were 13 employees out who were either positive for COVID or quarantined, up from two a couple weeks ago. Staffing is maintaining or reaching capacity. There are no extra ICU beds.
The CMOs briefing is online at https://us02web.zoom.us/rec/share/bHgC4w5z41OIQRZN9fqEyFHWxdsYe7RkdEb5qzRJSkfzE005J8hILcVGk6WWlJ0.sqlMzEa9u57RKz7h.
Free vaccines available
Free COVID-19 vaccines will be available from 10 a.m. to 6 p.m. Wednesday through Friday at the Kmart vaccination site, 7836 State Ave., Kansas City, Kansas. Vaccines are free for people ages 12 and older. There are gifts available, and a “Spin to Win” promotion is ongoing for Wyandotte County residents, as supplies last.
For more information on the Unified Government Health Department’s vaccine schedule, see WycoVaccines.org.
Mobile vaccines can still be requested online at WycoVaccines.org or by calling 3-1-1 (913-573-5311).
Other sites available for vaccinations
Free vaccinations at KU Health System are open to the public. Current patients may use MyChart to make an appointment. Others may call 913-588-1227 or visit kansashealthsystem.com/vaccine to make an appointment to get vaccinated. KU Health System currently is vaccinating residents of Kansas and Missouri who are 12 or older, by appointment only. Those under 18 must be accompanied by a parent or guardian throughout the appointment.
There are also pharmacies giving free COVID-19 vaccinations in Wyandotte County by appointment, when available. These include Price Chopper and Hen House pharmacies, which are now also accepting walk-in vaccinations or appointments, and are starting vaccinations for age 12 and up at those pharmacies that are giving Pfizer vaccine (see https://www.ballsfoodspharmacy.com/).
CVS has announced walk-in appointments for COVID-19 vaccine at some of its stores. Those interested in getting a vaccination at a CVS pharmacy are asked to visit a CVS website in order to make sure there is vaccine available. The website is at www.cvs.com/. Walgreens and Walmart also were listed on www.vaccines.gov as giving vaccinations.
Other pharmacies and sites giving vaccines are listed at www.vaccines.gov. The website also tells whether vaccines are in stock at the locations.
Case numbers reported
Wyandotte County reported a cumulative 20,625 cases on Friday, an increase of 85 since Thursday, according to the Unified Government Health Department’s COVID-19 webpage. There was a cumulative total of 312 deaths reported, an increase of two since Thursday.
On Wednesday, Aug. 4, the Unified Government Health Department reported that 42.36 percent of Wyandotte County residents had received at least one dose of vaccine. Those completing their vaccinations totaled about 35.87 percent.
The percentage of Wyandotte County residents who were age 12 and older who had received at least one dose was 52.1 percent.
The Kansas Department of Health and Environment reported 339,527 cumulative COVID-19 cases in Kansas on Friday, Aug. 6, an increase of 2,177 since Wednesday, Aug. 4. There was a total of 5,299 cumulative deaths reported statewide, an increase of 13 since Aug. 4.
The KDHE reported 64,508 cumulative COVID-19 cases in Johnson County on Aug. 6, an increase of 431 since Aug. 4. Leavenworth County had 8,207 cases, an increase of 77 since Aug. 4. Sedgwick County (the Wichita area) reported 60,963 cases, an increase of 355 since Aug. 4.
Free testing available
Free COVID-19 testing is available from 9 a.m. to 3 p.m. Monday through Friday at the UG Health Department’s central location, the former Kmart, 7836 State Ave., Kansas City, Kansas. Free gift cards are available to those who get a test, while supplies last.
Besides Health Department sites, COVID-19 testing is available at several locations in Wyandotte County.
Visit gogettested.com/Kansas and https://wyandotte-county-covid-19-hub-unifiedgov.hub.arcgis.com/pages/what-to-do-if-you-think-you-have-covid-19 for more sites.
Wyandotte County residents may contact the Health Department at wycohelp.org to sign up for a test to be delivered to their home.
For more details about free COVID-19 testing offered by the UG Health Department, visit https://wyandotte-county-covid-19-hub-unifiedgov.hub.arcgis.com/pages/what-to-do-if-you-think-you-have-covid-19, https://www.facebook.com/UGHealthDept or call 3-1-1.
